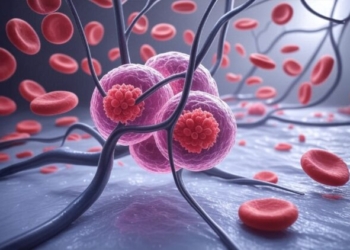
New York: Specific proteins in the blood of Covid-19 patients may help predict who may need to be placed on ventilators to breathe and which ones are most likely to die of the virus, according to a study.
The study led by researchers at Washington University School of Medicine in St. Louis showed that obtaining the samples early can help identify the proteins linked to worse Covid outcomes, accelerate treatment and prevent the need for ventilators or death from the virus.
“Identifying harmful proteins may be helpful as we confront not only variants of the virus that causes Covid-19, but also as new viruses emerge in the future,” said principal investigator Carlos Cruchaga, Director of the NeuroGenomics and Informatics Centre at the School of Medicine.
“We may be able to draw blood from an individual with a Covid infection, check the levels of these key proteins and quickly determine risk for serious outcomes. We then could use that information to determine the best course of treatment,” Cruchaga added.
For the study, published in the journal iScience, the team studied plasma samples from 332 Covid-19 patients admitted to Barnes-Jewish Hospital in St. Louis, and compared them to plasma samples from 150 people who had not been infected with SARS-CoV-2, the virus that causes Covid-19.
To study the proteins in the blood plasma, the researchers used a technique called high-throughput proteomics to identify overexpression and underexpression — also known as dysregulation — of the proteins.
The scientists conducted additional testing to distinguish which of the proteins actually caused severe illness from those that became dysregulated as a result of severe illness.
Although the research team identified a large number of proteins that were altered in patients with Covid-19, they determined that the presence of any of 32 proteins that become dysregulated during Covid infection indicated that patients would require breathing assistance from a ventilator.
They identified another five proteins that, when found to be altered in blood plasma as a result of the virus, indicated likelihood of death for the patient.
“Many of the proteins we identified were related to inflammation and to the body’s immune response, for example, so it wasn’t surprising to find them altered by Covid infection,” Cruchaga said. “But a subset of these proteins raised the likelihood that patients would need ventilation or go on to die. Using these proteomics approaches, we now have a methodology that allows us to predict problems, and that can be very important for clinical practice.”
To further test their findings, the researchers studied similar proteomics data from 297 Covid-19 patients and 76 controls at Massachusetts General Hospital in Boston and found that the same proteins indicated the eventual need for ventilators and the likelihood of death in both groups of patients.
(IANS)